When Doctors Make House Calls, Modern-Style!
Nearly half prefer in-person doctor visits, but telehealth boasts accessibility and disease avoidance benefits. Science examines quality, barriers, and elderly patient experiences in telemedicine.
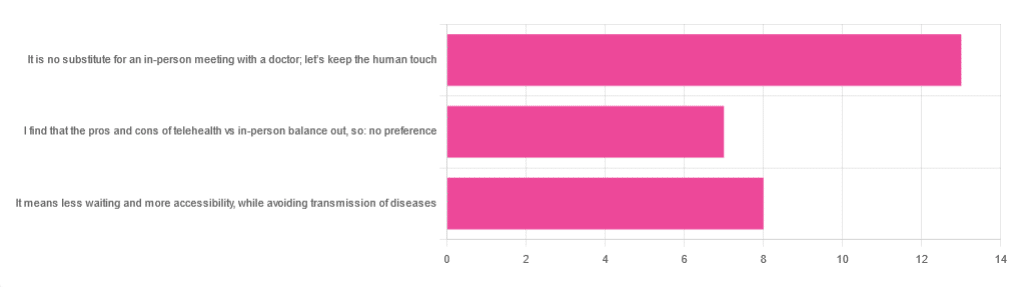
In Tuesday’s newsletter, we asked you foryour opinion of telehealth for primary care consultations*, and got the above-depicted, below-described, set of responses:
- About 46% said “It is no substitute for an in-person meeting with a doctor; let’s keep the human touch”
- About 29% said “It means less waiting and more accessibility, while avoiding transmission of diseases”
- And 25 % said “I find that the pros and cons of telehealth vs in-person balance out, so: no preference”
*We specified that by “primary care” we mean the initial consultation with a non-specialist doctor, before receiving treatment or being referred to a specialist. By “telehealth” we mean by videocall or phonecall.
So, what does the science say?
A quick note first
Because telehealth was barely a thing (statistically speaking) before the first stages of the COVID pandemic, compared to how it is now, most of the science for this is young, and a lot of the science simply hasn’t been done yet, and/or has not been published yet, because the process can take years.
Because of this, some studies we do have aren’t specifically about primary care, and are sometimes about specialists. We think this should not affect the results much, but it bears highlighting.
Nevertheless, we’ll do what we can with the science we have!
Telehealth is more accessible than in-person consultations: True or False?
True, for most people. For example…
❝Data was found from a variety of emergency and non-emergency departments of primary, secondary, and specialised healthcare.
Satisfaction was high among recipients of healthcare, scoring 9-10 on a scale of 0-10 or ranging from 73.3% to 100%.
Convenience was rated high in every specialty examined. Satisfaction of clinicians was high throughout the specialities despite connection failure and concerns about confidentiality of information.❞
whereas…
❝Nonetheless, studies reported perception of increased barriers to accessing care and inequalities for vulnerable patients especially in older people❞
~ Ibid.
Source: Satisfaction with telemedicine use during COVID-19 pandemic in the UK: a systematic review
Now, perception of those things does necessarily equate to an actual increased barrier, but it is reasonable that someone who thinks something is inaccessible will be less inclined to try to access it.
The quality of care provided via telehealth is as good as in-person: True or False?
True, ostensibly, with caveats. The caveats are:
- We’re going offreported patient satisfaction, not objective patient health outcomes (we found little* science as yet for the relative incidence of misdiagnosis, for example—which kind of thing will take time to be revealed).
- We’re also therefore speaking (as statistics do) for the significant majority of people. However, if we happen to be (statistically speaking) an insignificant minority, well, that just sucks for us personally.
*we did find some, but it wasn’t very helpful yet. For example:
An electronic trigger to detect telemedicine-related diagnostic errors
👆 this one does look at the incidence of diagnostic errors, but provides no control group (i.e. otherwise-comparable in-person consultations) for comparison.
While most oft-considered demographic groups reported comparable patient satisfaction (per race, gender, and socioeconomic status, for example), there was one outlier variable, which was age (as we quoted from that first study above).
However!
Looking under the hood of these stats, it seems that age is not the real culprit, so much as technological illiteracy, which is heavily correlated with age:
❝Lower eHealth literacy is associated with more negative attitudes towards I/C technology in healthcare. This trend is consistent across diverse demographics and regions. ❞
Source: Meta-analysis: eHealth literacy and attitudes towards internet/computer technology
There are things that can be done at an in-person consultation that can’t be done by telehealth: True or False?
True, of course. It is incredibly rare that we will cite “common sense”, (as sometimes “common sense” is actually “common mistakes” and is simply and verifiably wrong), but in this case, as one 10almonds subscriber put it:
❝The doctor uses his five senses to assess. This cannot be attained over the phone❞
~ 10almonds subscriber
A quick note first: if your doctor is using their sense of taste to diagnose you, please get a different doctor, because they should definitely not be doing that!
Not in this century, anyway… Once upon a time, diabetes was diagnosed by urine-tasting (and yes, that was a fairly reliable method).
However, nowadays indeed a doctor will use sight, sound, touch, and sometimes even smell.
In a videocall we’re down to two of those senses (sight and sound), and in a phonecall, down to one (sound) and even that is hampered. Your doctor cannot, for example, use a stethoscope over the phone.
With this in mind, it really comes down to what you need from your doctor in that consultation.
- If you’re 99% sure that what you need is to be prescribed an antidepressant, that probably doesn’t need a full physical.
- If you’re 99% sure that what you need is a referral, chances are that’ll be fine by telehealth too.
- If your doctor is 99% sure that what you need is a verbal check-up (e.g. “How’s it been going for you, with the medication that I prescribed for you a month ago?”, then again, a call is probably fine.
If you have a worrying lump, or an unhappy bodily discharge, or an unexplained mysterious pain? These things, more likely an in-person check-up is in order.
Take care!
Share This Post
Learn To Grow
Sign up for weekly gardening tips, product reviews and discounts.