Cannabis Myths vs Reality
Cannabis myths debunked: smoking it doesn’t cause lung cancer, edibles can be dangerous, and it’s not a gateway drug. Stay informed and stay safe.
Cannabis Myths vs Reality
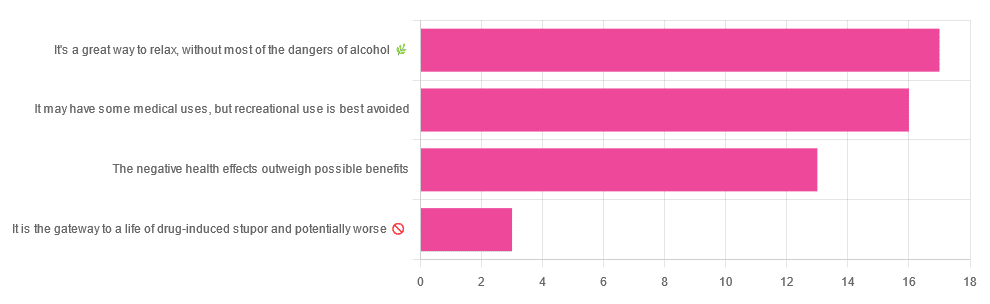
We asked you for your (health-related) opinion on cannabis use—specifically, the kind with psychoactive THC, not just CBD. We got the above-pictured, below-described, spread of responses:
- A little over a third of you voted for “It’s a great way to relax, without most of the dangers of alcohol”.
- A little under a third of you voted for “It may have some medical uses, but recreational use is best avoided”.
- About a quarter of you voted for “The negative health effects outweigh the possible benefits”
- Three of you voted for “It is the gateway to a life of drug-induced stupor and potentially worse”
So, what does the science say?
A quick legal note first: we’re a health science publication, and are writing from that perspective. We do not know your location, much less your local laws and regulations, and so cannot comment on such. Please check your own local laws and regulations in that regard.
Cannabis use can cause serious health problems: True or False?
True. Whether the risks outweigh the benefits is a personal and subjective matter (for example, a person using it to mitigate the pain of late stage cancer is probably unconcerned with many other potential risks), but what’s objectively true is that it can cause serious health problems.
One subscriber who voted for “The negative health effects outweigh the possible benefits” wrote:
❝At a bare minimum, you are ingesting SMOKE into your lungs!! Everyone SEEMS TO BE against smoking cigarettes, but cannabis smoking is OK?? Lung cancer comes in many forms.❞
Of course, that is assuming smoking cannabis, and not consuming it as an edible. But, what does the science say on smoking it, and lung cancer?
There’s a lot less research about this when it comes to cannabis, compared to tobacco. But, there is some:
❝Results from our pooled analyses provide little evidence for an increased risk of lung cancer among habitual or long-term cannabis smokers, although the possibility of potential adverse effect for heavy consumption cannot be excluded.❞
Read: Cannabis smoking and lung cancer risk: Pooled analysis in the International Lung Cancer Consortium
Another study agreed there appears to be no association with lung cancer, but that there are other lung diseases to consider, such as bronchitis and COPD:
❝Smoking cannabis is associated with symptoms of chronic bronchitis, and there may be a modest association with the development of chronic obstructive pulmonary disease. Current evidence does not suggest an association with lung cancer.❞
Read: Cannabis Use, Lung Cancer, and Related Issues
Cannabis edibles are much safer than smoking cannabis: True or False?
Broadly True, with an important caveat.
One subscriber who selected “It may have some medical uses, but recreational use is best avoided”, wrote:
❝I’ve been taking cannabis gummies for fibromyalgia. I don’t know if they’re helping but they’re not doing any harm. You cannot overdose you don’t become addicted.❞
Firstly, of course consuming edibles (rather than inhaling cannabis) eliminates the smoke-related risk factors we discussed above. However, other risks remain, including the much greater ease of accidentally overdosing.
❝Visits attributable to inhaled cannabis are more frequent than those attributable to edible cannabis, although the latter is associated with more acute psychiatric visits and more ED visits than expected.❞
Note: that “more frequent” for inhaled cannabis, is because more people inhale it than eat it. If we adjust the numbers to control for how much less often people eat it, suddenly we see that the numbers of hospital admissions are disproportionately high for edibles, compared to inhaled cannabis.
Or, as the study author put it:
❝There are more adverse drug events associated on a milligram per milligram basis of THC when it comes in form of edibles versus an inhaled cannabis. If 1,000 people smoked pot and 1,000 people at the same dose in an edible, then more people would have more adverse drug events from edible cannabis.❞
See the numbers: Acute Illness Associated With Cannabis Use, by Route of Exposure
Why does this happen?
- It’s often because edibles take longer to take effect, so someone thinks “this isn’t very strong” and has more.
- It’s also sometimes because someone errantly eats someone else’s edibles, not realising what they are.
- It’s sometimes a combination of the above problems: a person who is now high, may simply forget and/or make a bad decision when it comes to eating more.
On the other hand, that doesn’t mean inhaling it is necessarily safer. As well as the pulmonary issues we discussed previously, inhaling cannabis has a higher risk of cannabinoid hyperemesis syndrome (and the resultant cyclic vomiting that’s difficult to treat).
You can read about this fascinating condition that’s sometimes informally called “scromiting”, a portmanteau of screaming and vomiting:
Cannabinoid Hyperemesis Syndrome
You can’t get addicted to cannabis: True or False?
False. However, it is fair to say that the likelihood of developing a substance abuse disorder is lower than for alcohol, and much lower than for nicotine.
See: Prevalence of Marijuana Use Disorders in the United States Between 2001–2002 and 2012–2013
If you prefer just the stats without the science, here’s the CDC’s rendering of that:
Addiction (Marijuana or Cannabis Use Disorder)
However, there is an interesting complicating factor, which is age. One is 4–7 times more likely to develop a substance abuse disorder, if one starts use as an adolescent, rather than later in life:
Cannabis is the gateway to use of more dangerous drugs: True or False?
False, generally speaking. Of course, for any population there will be some outliers, but there appears to be no meaningful causal relation between cannabis use and other substance use:
Interestingly, the strongest association (where any existed at all) was between cannabis use and opioid use. However, rather than this being a matter of cannabis use being a gateway to opioid use, it seems more likely that this is a matter of people looking to both for the same purpose: pain relief.
As a result, growing accessibility of cannabis may actually reduce opioid problems:
- Cannabis as a Gateway Drug for Opioid Use Disorder
- Association between medical cannabis laws and opioid overdose mortality has reversed over time
Some final words…
Cannabis is a complex drug with complex mechanisms and complex health considerations, and research is mostly quite young, due to its historic illegality seriously cramping science by reducing sample sizes to negligible. Simply put, there’s a lot we still don’t know.
Also, we covered some important topics today, but there were others we didn’t have time to cover, such as the other potential psychological benefits—and risks. Likely we’ll revisit those another day.
Lastly, while we’ve covered a bunch of risks today, those of you who said it has fewer and lesser risks than alcohol are quite right—the only reason we couldn’t focus on that more, is because to talk about all the risks of alcohol would make this feature many times longer!
Meanwhile, whether you partake or not, stay safe and stay well.
Share This Post
Learn To Grow
Sign up for weekly gardening tips, product reviews and discounts.