Addiction Myths That Are Hard To Quit
Addiction myths debunked: Treatabiltiy revealed, cold turkey evaluated, and strategies like gradual reduction and substitution scrutinized with science-backed insights.
Which Addiction-Quitting Methods Work Best?
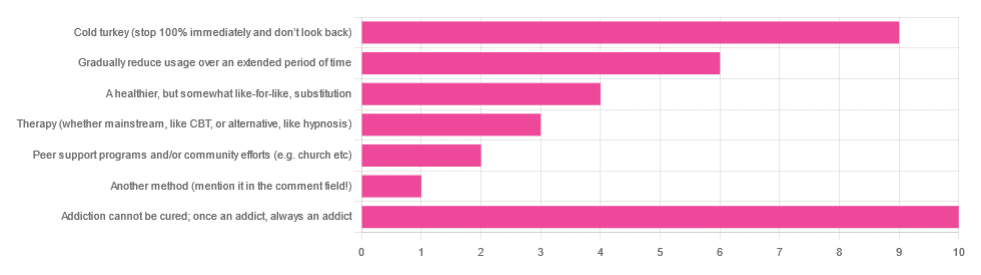
In Tuesday’s newsletter we asked you what, in your opinion, is the best way to cure an addiction. We got the above-depicted, below-described, interesting distribution of responses:
- About 29% said: “Addiction cannot be cured; once an addict, always an addict”
- About 26% said “Cold turkey (stop 100% and don’t look back)”
- About 17% said “Gradually reduce usage over an extended period of time”
- About 11% said “A healthier, but somewhat like-for-like, substitution”
- About 9% said “Therapy (whether mainstream, like CBT, or alternative, like hypnosis)”
- About 6% said “Peer support programs and/or community efforts (e.g. church etc)”
- About 3% said “Another method (mention it in the comment field)” and then did not mention it in the comment field
So what does the science say?
Addiction cannot be cured; once an addict, always an addict: True or False?
False, which some of the people who voted for it seemed to know, as some went on to add in the comment field what they thought was the best way to overcome the addiction.
The widespread belief that “once an addict, always an addict” is a “popular truism” in the same sense as “once a cheater, always a cheater”. It’s an observation of behavioral probability phrased as a strong generalization, but it’s not actually any kind of special unbreakable law of the universe.
And, certainly the notion that one cannot be cured keeps membership in many 12-step programs and similar going—because if you’re never cured, then you need to stick around.
However…
❝What is the definition of addiction?
Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences.
Prevention efforts and treatment approaches for addiction are generally as successful as those for other chronic diseases.❞
~ American Society of Addiction Medicine
Or if we want peer-reviewed source science, rather than appeal to mere authority as above, then:
❝What is drug addiction?
Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking and use despite adverse consequences. It is considered a brain disorder, because it involves functional changes to brain circuits involved in reward, stress, and self-control. Those changes may last a long time after a person has stopped taking drugs.
Addiction is a lot like other diseases, such as heart disease. Both disrupt the normal, healthy functioning of an organ in the body, both have serious harmful effects, and both are, in many cases, preventable and treatable.❞
~ Nora D. Volkow (Director, National Institute of Drug Abuse)
Read more: Drugs, Brains, and Behavior: The Science of Addiction
In short: part of the definition of addiction is the continued use; if the effects of the substance are no longer active in your physiology, and you are no longer using, then you are not addicted.
Just because you would probably become addicted again if you used again does not make you addicted when neither the substance nor its after-effects are remaining in your body. Otherwise, we could define all people as addicted to all things based on “well if they use in the future they will probably become addicted”.
This means: the effects of addiction can and often will last for long after cessation of use, but ultimately, addiction can be treated and cured.
(yes, you should still abstain from the thing to which you were formerly addicted though, or you indeed most probably will become addicted again)
Cold turkey is best: True or False?
True if and only if certain conditions are met, and then only for certain addictions. For all other situations… False.
To decide whether cold turkey is a safe approach (before even considering “effective”), the first thing to check is how dangerous the withdrawal symptoms are. In some cases (e.g. alcohol, cocaine, heroin, and others), the withdrawal symptoms can kill.
That doesn’t mean they will kill, so knowing (or being!) someone who quit this way does not refute this science by counterexample. The mortality rates that we saw while researching varied from 8% to 37%, so most people did not die, but do you really want (yourself or a loved one) to play those odds unnecessarily?
See also: Detoxification and Substance Abuse Treatment
Even in those cases where it is considered completely safe for most people to quit cold turkey, such as smoking, it is only effective when the quitter has appropriate reliable medical support, e.g.
- Without support: 3–5% success rate
- With support: 22% success rate
And yes, that 22% was for the “abrupt cessation” group; the “gradual cessation” group had a success rate of 15.5%. On which note…
Gradual reduction is the best approach: True or False?
False based on the above data, in the case of addictions where abrupt cessation is safe. True in other cases where abrupt cessation is not safe.
Because if you quit abruptly and then die from the withdrawal symptoms, then well, technically you did stay off the substance for the rest of your life, but we can’t really claim that as a success!
A healthier, but somewhat like-for-like substitution is best: True or False?
True where such is possible!
This is why, for example, medical institutions recommend the use of buprenorphine (e.g. Naloxone) in the case of opioid addiction. It’s a partial opioid receptor agonist, meaning it does some of the job of opioids, while being less dangerous:
It’s also why vaping—despite itself being a health hazard—is recommended as a method of quitting smoking:
Similarly, “zero alcohol drinks that seem like alcohol” are a popular way to stop drinking alcohol, alongside other methods:
This is also why it’s recommended that if you have multiple addictions, to quit one thing at a time, unless for example multiple doctors are telling you otherwise for some specific-to-your-situation reason.
Take care!
Share This Post
Learn To Grow
Sign up for weekly gardening tips, product reviews and discounts.